SKIN CANCER (Melanoma & Sentinel lymph node dissection, Squamous cell carcinoma, Basal cell carcinoma)
Skin cancer comprises lesions of different origin that require individualized treatment, according to their degree of malignancy. The patient might be advised to consult an oncologist in some cases of Malignant Melanoma or Squamous Cell Carcinoma. The most common categories of skin and soft tissue neoplasms are:
A) Basal cell carcinoma: The most common type of skin cancer worldwide. The treatment of choice is surgical excision to healthy borders. The possibility of metastases is really low (0.1%).
B) Squamous cell carcinoma: The 2nd most common skin cancer type. The treatment comprises surgical excision and follow up (according the individual characteristics of the tumor) for 3-5 years. Any further complementary examination (CT, MRI, pet scan) or treatment (e.g. irradiation) needed is decided after evaluation of the oncologist. The rate of distant metastases is 6%.
C) Melanoma: It’s advised that dermoscopically suspicious for melanoma lesions should not be partly biopsied but with excisional biopsy ( close to the lesion but total removal). This is safer as concerns cancer cell spreading. According the histology report the rest of treatment is defined according the type and staging of Melanoma. The tumor thickness is decisive on the extent of wide local excision and sentinel lymph node biopsy.
D) Rest types of skin cancer with more rare incidence: neuroendocrine carcinoma (Merkel cell carcinoma), keratoacanthoma, atypical fibroxanthoma etc.
Ε) Sarcoma: Dermatofibrosarcoma protuberans, Kaposi sarcoma, leiomyosarcoma, angiosarcoma.
Operation
Wide local excision of the lesion and plastic reconstruction of the defect. The reconstruction options include:
Immediate closure (when skin laxity allows).
Full thickness skin graft (rarely partial thickness skin graft) from another body part that resembles the characteristics of the the defect. The donor area is sutured primarily. Intra-operative tissue expansion to achieve decreased tension closure.
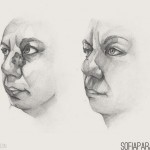
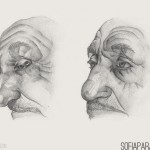
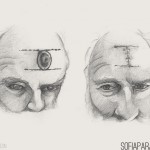
Local flap. A flap is a piece of tissues (skin, subcutaneous fat, fascia, muscle, bone) planned to rotate or advance into the defect from an adjacent area.
Secondary intention closure: In cases of small defects in specific anatomic areas (e.g. nose tip, inner canthus, scalp) it is less disfiguring to let the wound heal by itself with frequent changes of dressings.
Distant flap: When the defect is of considerable size or is comprised of different types of tissues, it needs to be replaced by a free flap. This is taken by another part of the body together with its feeding vessels and nerve. It is transferred to the area of the defect and the vessels and nerve are joined with corresponding structures of the recipient area.
Sentinel lymph node biopsy and lymph node dissection
In some cases of melanoma and squamous cell carcinoma selectively, the criteria indicating high risk of lymph node involvement are met. In those cases it’s suggested to undergo sentinel lymph node biopsy. The procedure is as follows: Radioisotope “marking” of the first lymph node that drains the lymph from the area of the excised melanoma.
A lymphophilic radioisotope is injected in the area of the scar from the excisional biopsy of the melanoma, on the skin. After few minutes we scan the anatomical area of the nearest group of lymph nodes and locate the 1st lymph node that receives the radioisotope. This is the sentinel lymph node.
The procedure is carried out in the nuclear medicine department of the hospital. Then you are transferred to the operation theatre. Before the start of the operation we inject a blue dye in the area of the scar that will follow lymph drainage and color the sentinel lymph node blue. After that we make a small incision in the area marked by the nuclear medicine doctor and by the aid of a specialized probe we trace the lymph node with most oscillations, which should also be colored blue.
The fact that a lymph node is marked by the radioisotope or the blue dye, DOES NOT mean that it is infiltrated by melanoma cells. It only means that if melanoma cells would leave the primary area of the skin, this lymph node would be their first stop. If the sentinel lymph node is infiltrated or not by melanoma is answered by the pathologists and the histology report after examining it microscopically.
If the sentinel lymph node is not involved, then you enter our follow up program by the oncologist and/or dermatologist. If it is involved, the lymph node’s area needs to be cleared completely e.g. axilla, groin, neck.
The major complication of lymph node dissection is lymphedema in 35% of cases. This occurs because the lymph cannot drain anymore from the area and this leads to lymphatic fluid pooling and swelling.
Restrictions and complications
The local excision of a, macroscopically considered malignant, lesion is done together with a healthy tissue border of 3-10mm because of the possibility of microscopic invasion of tumor cells around the area of the lesion. If the neoplasm is in an anatomically sensitive area (nose tip, eyelid, lip) there is the possibility that the aesthetic result will be compromised by the oncologic result. Small defects will be corrected after complete wound healing. Secondary corrections are very common in skin cancer surgery.
The mean value of operations when treating skin cancer is 2 and the reason is mainly to achieve the most satisfactory aesthetic result. Possible complications include wound dehiscence, hematoma (blood collection under the skin), and wound infection. In the case of free flap surgery the most serious complication is total or partial loss of the transplanted part and it’s usually attributed to compromised blood flow, comorbidities (diabetes mellitus, smoking, hypertension, vascular disease) and inadequate surgical technique.
After the operation
In most cases you can be discharged from the hospital the next day after the surgery, but you have to remain indoor for 2 days and in calmness. It’s advised not to wet the wound for 24 hours and for the next days it should be covered by a waterproof adhesive when you take a shower.
Suture removal is done on the 10th-15th day depending on the area that was operated. In cases of more complex reconstructions with free flap, you have to stay hospitalized for about 1 week.
In any case, after these kinds of operations you will have 1 or 2 drains that will be removed when the fluid collected decreases to <50ml.